Distrust, the vaccine and COVID-19
Written by Professor Nick Emmel
In this post, Nick Emmel discusses why a sociological understanding of trust is so important as vaccines for COVID-19 become available.
Credit: NIAID-RML_accessed wikimedia.org
I KNOW where I was when the paper confirming the safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2, the Oxford—AstraZeneca COVID-19 vaccine, was published. I was giving a live talk on inequalities in health and the COVID-19 pandemic through the medium of a computer streaming tool. A message appeared in the chat bar. I glanced at it but didn’t take it in. Many of us who have been obliged to transition to teaching on-line have got used to the multi-tasking environment of live-streaming apps. But teaching and chatting are two different things, even in these on-line environments designed to bombard participants with a deluge of multiple streams of information. So, instead of weaving the important news into my talk that we have a peer-reviewed and trustworthy account of a preliminary analysis of the safety of a vaccine administered to participants in the UK, South Africa and Brazil, I carried on talking about inequalities in health and why we should really think hard about distrust, where it comes from and how we might address it.
Distrust and vaccines dance around each other. The publication of Andrew Wakefield’s paper in 1998 in the Lancet claiming a causal link between the measles, mumps and rubella (MMR) vaccine and autism, since repudiated and expunged from the journal where it was published, gave anti-vaxxers newfound energy. Old stories about failed batches of polio vaccine have been reinvigorated and new stories invented about claims made through the National Vaccine Injury Compensation Program in the United States. These vastly over-inflate its caseload. They stoke conspiracy theories that feed the embers of distrust. In the United Kingdom stories in a local paper in South West Wales about unsafe vaccines was effective enough to reduce immunisation levels of the MMR vaccine to well below the level required for herd immunity. This was a public health emergency. The R rate, with which we have all become so familiar, is much, much higher than for COVID-19. Measles is virulently infectious, and it kills. Public health officials desperate to get the vaccination level up reported being told to mind their own business when they asked if children had been immunised. It took a huge amount of work convincing parents to get vaccination back to a safe level in the community.
My talk about inequalities in health did not touch on the anti-vaxxers at all. The outcomes of their senseless campaigns cause suffering, but they don’t explain the gradients of health I was talking about. When the message about the safety and efficacy of the COVID-19 vaccine popped up in the chatbox I was talking about someone else from South Wales, a general practitioner, health researcher and activist called Julian Tudor-Hart. Tudor-Hart knew, firsthand, about inequalities in health. He worked in Glyncorrow in the Afan Valley, where many of the patients in his practice were coal miners and their families. His patients lived disabled and shorter than average lives. Based on some good field-based shoe leather epidemiology he came up with a compelling idea he called the Inverse Care Law—those most in need of care are least likely to access it. My talk located distrust seen through the lens of Tudor-Hart’s Inverse Care Law far, far more than in strange dreamt up notions of anti-vaccination.
Thanks to the shoe-leather epidemiology of Tudor-Hart and very many others we know a lot about inequalities in health in the United Kingdom. Administrative data does not provide such a detailed picture anymore. Like in England and Wales, in the city in which I was doing my virtual talk, Leeds, the increase in life expectancy for men has stalled and for women over the age of 80 years old was in decline before the COVID-19 pandemic. Explaining these trends is made difficult because fine-grained data at an administrative ward level is not readily available through the public health observatories these days. This is a political decision, no doubt. The most recent data available at this granular level is in the Director of Public Health Report of 2012. Women in one of the poorest wards in Leeds might expect, on average, to live to 75 years old while her fellow Loiner in a richer ward in the suburbs might live, on average, to 88.6 years. For men, the difference is much more stark. Life expectancy for men is 64.2 years in one of the poorest wards and 82 years in the richest ward; a difference of 17.8 years of life in 13.7 miles travelled from near the city centre to its leafy and wealthy suburbs.
Without an annual reminder of these differences in life expectancy in the reports of Directors of Public Health—these gradients are similar between the richest and poorest administrative wards across all the major cities of the UK—discussions about these unfair differences faded from public discourse. They were replaced with discussions about the cause of aggregate changes in life-expectancy. One side individualised the problem and blamed the flu and the other the patterns of deprivation still visible in the numbers, albeit the comparison was now between poor Blackpool and rich Poole in Dorset. Both sides agreed with the Office for National Statistics and the pension actuaries that life expectancy at birth was stalling and even going into decline. Then the COVID-19 pandemic struck and once again the fine-grained contrast in life experience between deprived groups and their less deprived neighbours were brought into focus.
The Intensive Care National Audit and Research Centre conducts an ongoing audit of intensive care and high dependency critical care bed occupancy across the NHS in England, Wales and Northern Ireland. Their regular reports showed that at the peak of the first wave on the COVID-19 pandemic in April and May, a rather large and heterogeneous group, classified in statistical reports as Black, Asian and Ethnic Minority (BAME), appeared to be occupying a disproportionate number of critical care beds. Mortality figures showed a similar pattern. It was hard not to associate these figures with deprivation and experiences associated with this deprivation such as working in unsafe jobs like front-line care work, relying on unsafe public transport and living in multiple-occupancy households. A report commissioned by the Chief Medical Officer, Chris Whitty and written by Professor Kevin Fenton and colleagues for Public Health England made similar observations about both the numbers and experiences of those affected by COVID-19 in this classificatory group (Paul Bagguley has written recently in this blog about the limitations of the BAME classification). More recently, in early December in the second wave of the pandemic, the Intensive Care National Audit and Research Centre continues to report steep gradient across levels of deprivation; 11.7% of patients critically ill with COVID-19 are in the least deprived fifth of the population, while 34.8% are from the most deprived fifth.
Back in July in a Parliamentary debate, Lord Reith quizzed Lord Bethell of Romford, Parliamentary Under-Secretary of State at the Department of Health and Social Care about figures released the month before by the Office for National Statistics. Those living in poor areas were 1.375 times more likely to die from COVID-19 than those living in richer areas. Could the noble lord explain this? Lord Bethell replied in a suitably contrite manner. Indeed it was a sensitive matter, he noted, that those living in poor areas were more likely to die from COVID-19. They were hardest hit by very many other diseases too. Lord Bethell went on to explain this was because of behavioural reasons, the decisions (poor) people make about social distancing and their own health.
Clare Bambra, a leading academic of inequalities in health followed by the editor of a leading medical journal, has suggested that COVID-19 should be thought of as a syndemic pandemic. The term syndemic was coined by the American epidemiologist Merrill Singer to describe the relationship between HIV/AIDS, substance abuse and violence. It is a set of closely intertwined and mutually enhancing health problems that significantly affect the overall health status of a population. COVID-19 brings existing inequalities in health into sharp relief. Lord Bethell emphasises this point. A syndemic also brings into focus explanations for the patterns of infection of COVID-19. These are, most likely, the same mechanisms that shape wider inequalities in health. There is nothing special about this virus in this regard. In explaining these patterns of inequality of COVID-19, Lord Bethell chose to focus on behaviour.
Limiting explanation about inequalities in health to behaviour and constitution, the characteristics and choices of individuals ignores more compelling explanations of inequalities in health, which again rely on robust shoe-leather epidemiology. Since 1985 a longitudinal study has been conducted with civil servants in Whitehall regularly recording very many measures of health, health problems and, because it has been going long enough, causes of death. This longitudinal study shows that even if genetic factors (evaluated through parenteral health records) and indicators of general health like blood pressure, Body Mass Index, cholesterol level and even smoking are statistically isolated, ‘controlled for’ in the jargon, junior civil servants are 2.1 times more likely to die of a heart attack before their 65th birthday than senior civil servants. Explanations for inequalities in health require a rather richer explanation than just constitutional and behavioural factors.
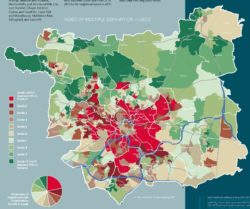
Index of Multiple Deprivation for Leeds source: Annual Report of the Director of Public Health 2017/18
The map of Leeds looks a little like a Yorkshire dartboard, which has a single bull and no triple ring around its middle. The centre, gentrified since the industrial decline of the 1980s, is surrounded by areas of high deprivation. These are the persistent sites of slums, recorded by Sanitation Commissioners in the 1840s, replaced with back-to-back housing and local authority housing more recently. A little further out are robust semi-detached social housing that accompanied slum clearance between the wars and the concrete mix of low and high rise housing built in the post-war social contract. These are areas of significant deprivation too. The tailoring, dyeing and mining industry these estates serviced left town in the 1980s. Interleaving these areas of deprivation are the homes of more affluent groups in the semi-detached suburbs of the city. The hub and spoke transport system that allowed the wealthier to flee their town-house residences in preference for the cleaner air of the suburbs still carries the most affluent residents of Leeds the 13.7 miles from its centre to the municipal border.
A map of the index of multiple deprivations imprinted on the city’s geography displays a dark doughnut of deprivation at its core, the lighter tones of affluence at its periphery. In 2004, when health data was disaggregated by administrative ward it was possible to map health conditions to this fine grain of inequalities too. A measure like death from a heart attack before the age of 65 years followed a similar pattern to the map of deprivation. People living in the areas of high deprivation were far more likely to suffer a heart attack than those living in areas of relative affluence. Yet, as two public health researchers found through investigating hospital admission records, those living in the least deprived suburbs and experiencing the least deaths from heart disease were far more likely to have interventions to address heart disease such as heart surgery, angioplasty and stents in their coronary arteries. Julien Tudor Hart’s inverse care law is working well in Leeds, it appears.
A few years ago, I sat talking with some community activists in a club in one of the slum clearance communities built between the wars. Rob had been a trade union organiser and fitter at Burton’s, a huge tailoring factory, makers of demob and wedding suits until it shut down in 1984. He didn’t have a proper job after that. He’d been waiting a long time for heart surgery. ‘I’ll die before I get it’, he observed ruefully. ‘It’s the way it is for us. You can’t trust ‘em to care for us’. Rob’s story isn’t unusual. It is one I’ve heard in my research in low-income areas in Leeds very many times. It might not be heart disease, it could be another illness, aches and pains that can’t get treated, or something else that affects the narrator’s health, maybe a broken water heater, rat infestation, garbage building up in the garden, benefits not being paid or incorrectly paid, children bullied at school, feeling unsafe on your own street. Hear these stories and it is easy to think about the individual telling them as the problem. Or you can listen in on these stories and hear something quite different.
Two researchers in Toxteth, a deprived area of Liverpool, sat in a doctor’s surgery and listened to the interactions between doctor and patient. What they heard were patients who ‘don’t want to bother the doctor’. What they saw were patients with multiple health problems who don’t present with textbook definitions of illness and are misdiagnosed. Remember lives are not just shorter in low-income areas, people live more of their lives with disability. And they witnessed cultural gaps and communication difficulties despite all but one patient having English as their first language. Doctors simply did not understand what their patients were saying, and the patients were confused too.
What these researchers found and what can be heard in the stories I’ve heard in my research is a yawning gap between those who deliver services, not just doctors, and those who draw on these parred down services in low-income areas. This means, simply, they don’t access the services they need to be healthy. If this is the repeated experience of health providing services, it is hard to rely on these services or have confidence in those who deliver them. Services and those who provide them are distrusted.
I got to the end of my talk. The moderator drew my attention to the note he had typed in the chat bar about the paper reporting on the safety of Oxford—AstraZeneca COVID-19 vaccine. That’s good, I thought, no more do we have to rely on press releases and social media prepared by the publicity department at AstraZeneca, we now have the paper to read and evaluate. For many, this scientific process will be enough to have trust in the vaccine. Based on my reading I’ve recommended my nearly nonagenarian Mum and Dad get the vaccine. But, for those most in need of the vaccine they are least likely to get it.
There is considerable distrust between service providers, who have the key job of promoting the safety and efficacy of a vaccine for COVID-19 and people who experience inadequate services in deprived communities. This distrust is certainly made worse through uncertainties about the safety of vaccines, promoted as conspiracy theories to groups who are distrustful of those who they see as having the power to deliver the services they need to be healthy and most often failing to do so (for an excellent overview of the conspiracy theories currently washing around the COVID pandemic along with their key proponents see https://www.covidfaq.co/).

Credit: Joel Rodrigues/Agência Brasília accessed wikimedia.org
Solutions to ensuring universal vaccination being discussed at the moment to address the challenges of distrust seem so narrow. They mainly focus on celebrity as the solution. A celebrity like Marcus Rashford, the Manchester United footballer who has confronted politicians and highlighted the real and lived experiences of material poverty, might have an impact. He understands the experiences of those who do not trust politicians or service providers. But we need to think more broadly. Trustful relations must be built in the context of vulnerabilities. These require more than a celebrity endorsement. They need a focus on building trustful relations through directly addressing the experiences of materially deprived individuals and groups whose experience is of repeated failures to adequately access the services they need to be healthy. This requires comprehensive solutions to addressing the health of those most unequal in our society. Otherwise, the prospect is of a continued syndemic—COVID-19 as one more health problem in the intertwined, interactive and cumulative experience of existing inequalities in health.
Further reading
Bambra C. et al. (2020) The COVID-19 pandemic and health inequalities. Journal of Epidemiology and Community Health
Ferrie J. E et al (2001) Employment status and health after privatisation in white collar civil servants: prospective cohort. British Medical Journal, 322, 647.
Ferrie J E et al (1995) Health effects of anticipation of job change and non-employment: longitudinal data from the Whitehall II study. British Medical Journal, 311, 1264-1269.
Hiam, L. & Dorling, D. (2018) Rise in mortality in England and Wales in first seven weeks of 2018. British Medical Journal, 360.
Tudor Hart J 1971, The Inverse Care Law, The Lancet pp. 405-412.
Wakefield A J et al. (1998) Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. The Lancet 351:637-641 RETRACTED
